Herniated or Ruptured Disc
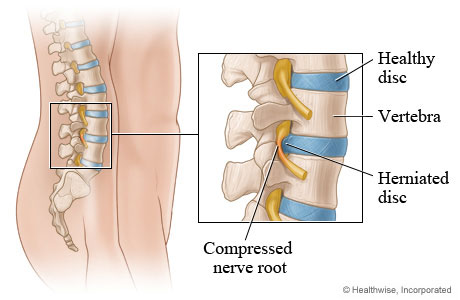
The bones of the spine are cushioned by discs, which are round and flat with a tough, outer shell (capsule) that surrounds a jelly-like material (nucleus).  When discs are healthy, they act as shock absorbers for the spine, keeping the spine flexible. When discs are damaged by injury, disease or the normal wear and tear associated with aging, they may bulge or rupture, becoming a herniated disc (sometimes called a slipped or ruptured disc).
Although injury to the outer covering of a disc can cause pain, often a herniated disc by itself does not cause any discomfort. Pain occurs when the herniated disc material presses on the nerve roots or spinal cord. Pain or numbness may occur in the area of the body affected by the nerve. For example, a herniated disc that presses on one of the nerve roots of the large nerve that extends from the lower back down the back or side of the leg may cause pain and numbness in the leg (a condition called sciatica).
When discs are healthy, they act as shock absorbers for the spine, keeping the spine flexible. When discs are damaged by injury, disease or the normal wear and tear associated with aging, they may bulge or rupture, becoming a herniated disc (sometimes called a slipped or ruptured disc).
Although injury to the outer covering of a disc can cause pain, often a herniated disc by itself does not cause any discomfort. Pain occurs when the herniated disc material presses on the nerve roots or spinal cord. Pain or numbness may occur in the area of the body affected by the nerve. For example, a herniated disc that presses on one of the nerve roots of the large nerve that extends from the lower back down the back or side of the leg may cause pain and numbness in the leg (a condition called sciatica).
Many people who have a herniated disc are not aware of it because they have no symptoms of leg or back pain. Symptoms that do appear vary greatly, depending on the position of the herniated disc. If the herniated disc is:
- Not pressing on a nerve, there may be a low backache or no symptoms at all
- Pressing on a nerve, pain or numbness can occur in the area of the body leading from the nerve
- Located in the neck, pain or numbness may be felt in the shoulders, arms, hands or chest
- Located in the lower back, sciatica may occur and cause leg pain and other nerve-related symptoms, such as weakness, numbness or tingling in one leg. Pain from a herniated disc in the lower back (sciatica) may be felt in the buttock and down the back or side of the leg to the ankle or foot. There may be low back pain, but it is usually not as severe as leg pain
 Nerve-related symptoms of a herniated disc include
Nerve-related symptoms of a herniated disc include
- Tingling ("pins and needles" sensation) or numbness in one leg that can begin in the buttock or behind the knee and extend to the ankle or foot
- Severe deep muscle pain and muscle spasms.
- Weakness in certain muscles in one or both legs
- Weakness in both legs and the loss of bladder and/or bowel control, which are symptoms of a specific and severe type of nerve root compression called cauda equina syndrome. This is a serious problem that requires immediate medical help
Herniated discs are caused by aging, degeneration of the disc (degenerative disc disease - DDD) or injury to the spine. Disc disease may result from tiny tears or cracks in the outer capsule of the disc, called the annulus. The jelly-like material inside the disc (nucleus) may be forced out through the tears or cracks in the capsule. This causes the disc to bulge, break open or break into sections. Disc disease may develop as part of the normal aging process. After about age 30, the nucleus of a spinal disc begins to lose its fluid content, becoming less springy and more easily injured. Herniated discs can affect people of all ages, but they are most common in people between 35 and 45 years old who perform heavy manual labor or drive motor vehicles for long periods of time. Herniated discs can occur anywhere in the spine, but most occur in the lower back or in the neck region.
Injury to the spine can occur from:- A sudden heavy strain or increased pressure to the lower back. Sometimes a sudden twisting movement or even a sneeze will force some of the jelly-like material inside the disc out through the disc's outer shell.
- Activities that are done over and over again that may stress the lower back, including poor lifting habits, bad sitting posture,prolonged exposure to vibration or sports-related injuries
For patients with leg and back >pain, the doctor may take a medical history and conduct a physical exam to determine whether symptoms might be caused by a herniated disc. X-rays may show a decrease in space between the vertebra indicating some sort of disc problem (discs are soft tissue and therefore are not seen well on X-ray). However, if the doctor suspects that there is a more serious underlying condition (such as a tumor, infection or severe nerve damage), or if leg pain and other symptoms do not get better after two to four weeks of nonsurgical treatment, X-rays may be taken. Electromyography (EMG) can be used to diagnose certain nerve and muscle disorders and may be done for people who have signs of prolonged pressure on a nerve root. However, results of this test will not determine if a herniated disc is causing the nerve root compression. A magnetic resonance imaging (MRI) scan may be done to confirm the location and seriousness of a herniated disc or to look for another condition, such as an infection or tumor. An MRI provides detailed images of the soft tissues of the spine, such as the muscles, tendons, ligaments and discs. Computed tomography (CT) scans may also be done to provide detailed images of bony structures of the spine. Other tests, such as blood tests, may also be done to rule out other conditions.
The SolutionWhite Sands Physical Therapy and Aquatics offers a protocol which combines computerized decompression tables, aquatic decompression and exercises, manual therapy and McKenzie extension exercises. This protocol can decrease bulging and herniated discs in most cases relieving back pain and radiating (pain that shoots down the leg) pain.


